Esophageal Manometry
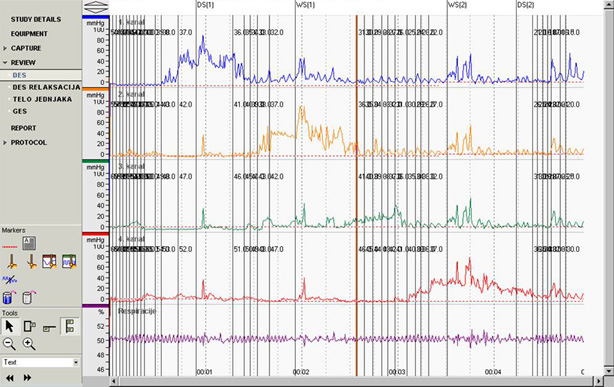
Esophageal manometry (EM) or an esophageal motility study (EMS) is a test to assess motor function of the upper esophageal sphincter (UES), esophageal body and lower esophageal sphincter (LES).
An EM is typically done to evaluate suspected disorders of motility or peristalsis of the esophagus. These include achalasia, diffuse esophageal spasm, nutcracker esophagus and hypertensive lower esophageal sphincter. These disorders typically present with dysphagia, or difficulty swallowing, usually to both solids and liquids even initially. Other patients with spasm disorders may have the test done to diagnose chest pain thought not to be of cardiac cause.
The test is not useful for anatomical disorders of the esophagus (that is, disorders that distort the anatomy of the esophagus), such as peptic strictures and esophageal cancer.
A catheter is placed into the nose and guided into the stomach. Once placed, the catheter is slowly withdrawn, allowing it to detect pressure changes and to record information for later review. The patient will be asked at times to take a deep breath or to take some swallows of water. The degree of discomfort varies among patients. Patients are not sedated because sedatives would alter the functioning of the esophageal muscles. Overall the procedure takes about 20 minutes. After the procedure is complete, patients can usually resume their normal daily activities.
Recently, high resolution manometry (HRM) has been developed that significantly reduces the procedure time and provides enhanced patient comfort. Newer catheters incorporate concurrent impedance with HRM.
What is esophageal manometry, and why is it performed?
Esophageal manometry measures the pressures and the pattern of muscle contractions in your esophagus. Abnormalities in the contractions and strength of the muscle or in the sphincter at the lower end of the esophagus can result in pain, heartburn, and/or difficulty swallowing. Esophageal manometry is used to diagnose the conditions that can cause these symptoms.
How should I prepare for esophageal testing?
An empty stomach allows for the best and safest examination, so do not eat or drink anything for 6 hours before the test. Since many medications can affect esophageal pressure and the natural muscle contractions required for swallowing, be sure to discuss with your healthcare professional each medication you are taking. Your doctor may ask that you temporarily stop taking one or more medications before your test.
What can I expect during and after the test?
A healthcare professional will apply a cream to numb the inside of your nostrils. Then a thin, flexible, lubricated tube will be passed through your nose and advanced into your stomach while you swallow sips of water. Mild, brief gagging may occur while the tube is passed through the throat. When the tube is in position, you will be sitting upright or lying on your back while the tube is connected to a computer. Once the test begins it is important to breathe slowly and smoothly, remain as quiet as possible and avoid swallowing unless instructed to do so. As the tube is slowly pulled out of your esophagus, the computer measures and records the pressures in different parts of your esophagus.
During the test, you may experience some discomfort in your nose and/or throat. The test will take approximately 30 minutes to complete and the results will be sent to your doctor’s office.
After the test, you may experience mild sore throat, stuffy nose, or a minor nosebleed; all typically improve within hours. Unless your physician has given you other instructions, you may resume normal meals, activities, and any interrupted medications.
What are the possible risks associated with esophageal manometry?
As with any medical procedure, there are certain risks. While serious side effects of this procedure are extremely rare, it is possible that you could experience irregular heartbeats, aspiration (when stomach contents flow back into the esophagus and are breathed into the lung), or perforation (a hole in the esophagus). During insertion, the tube may be misdirected into the windpipe before being repositioned. Precautions are taken to prevent such risks, and your physician believes the risks are outweighed by the benefits of this test.
What if the tube cannot be passed?
In some situations, correct placement of the tube may require passage through the mouth or passing the tube using endoscopy (a procedure that uses a thin, flexible lighted tube). Your physician will determine the best approach.
Understanding Esophageal Manometry.
American Society for Gastrointestinal Endoscopy 2015. ©
Diagnostics
- Medical History
- Abdominal Ultrasound
- Upper GI Series
- Upper GI Endoscopy
- Esophageal Manometry
- Esophageal 24-Hour pH Metry
- Esophageal 24-Hour pH Impedance
Lexicon
Patients Informations
Soon
If you have more questions contact us:
info@refluxcentar.com

 српски
српски