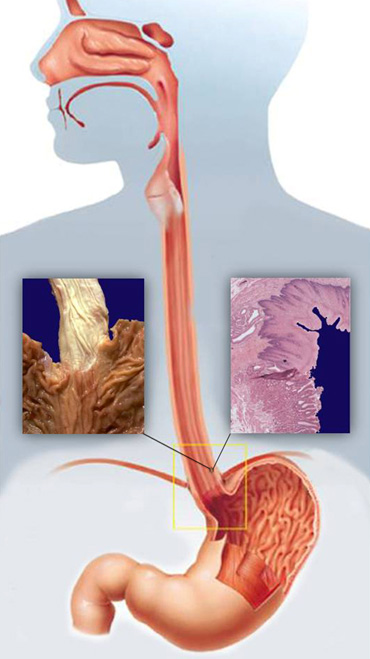
The digestive tract (the system of the digestive or gastrointestinal tract) consists of a number of authorities which are taking place in stages of digestion and absorption. The digestive tract to continuous supplies the organism with water, electrolytes and food, and to achieve this it isnecessary to the normal movement of fluids and food, the secretion of digestive juices and food, absorption of products of digestion, as well as control of all these functions, the nervous and hormonal systems. The boundary between the upper and lower part of the digestive tract represents duodenal suspensory ligament also known as Treitz’s ligament. Anatomical and functional point upper digestive tract consists of the mouth, pharynx, esophagus, stomach and duodenum. The oral cavity has the function of receiving food. In the oral cavity are extra digestive organs: teeth, tongue and salivary glands. The esophagus is defined as muskulomembranozni tube that conducts food from the throat to the stomach. The main roles of the esophagus are swallowed implementation of solid and liquid food in the stomach and preventing the recurrence of gastric contents, while the role of secretory and absorptive scarce negligible. These functions are realized esophagus precise combination of muscle and body two sfinkterna mechanism, the upper (GES) and the lower esophageal sphincter (DES). The normal function of the body of the esophagus is achieved through peristaltic contraction, which in coordination with both premature relaxation of the sphincter. The word esophagus is the Greek etymology (oisophagos) and consists of two parts: oisein words carry meaning, and words phagos, which means to eat or phagema which means food. The etymology of the Greek noun sphincter (sphincter), and its semantics is a wire or string, or the one that tightens. In the stomach, in terms of high acidity occurs biochemical degradation of food. In duodenal ulcer thus digested food comes into contact with enzymes of the liver and pancreas, which further facilitates the breakdown and absorption of food, but in the small intestine.
Anatomy
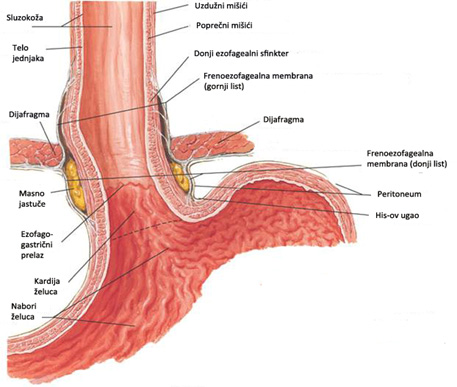
Anatomically and functionally esophagus can be divided into three main segments: cervical, thoracic and abdominal. The origin of the esophagus is located in the neck, and mostly it is positioned in the back of the chest, while the final part of the esophagus is located in the abdominal cavity. Length of the esophagus is anatomically defined as the distance between the top edge of the upper esophageal sphincter (muscle krikofaringealnog) and the lower edge of DES. The esophagus is an average of 28 cm long, and between about 30 wide x 20 mm. The esophagus has gone into the abdominal cavity through the opening in the diaphragm, which is called jednjačni opening (esophageal hiatus). At the level of the diaphragm, the esophagus is surrounded by collagen and elastic fibers so. frenoezofagealnom membrane. Belly deo esophagus varies in length from 3 and 5 cm (average about 3.5 cm), and there is a hiatus from the esophagus to the point at which connects with the stomach or esophagogastric transition (EEA). The pressure in the chest cavity is below the level of the atmospheric pressure (-6 mm Hg), and at the abdominal always above (+6 mm Hg), whereby this difference in pressures is actively contributing to the normal function of the body of the esophagus and DES.
Adequate physiology of the esophagus caused by the specific structure of its muscular layer and innervation, but also the uniqueness of his anatomy. The muscle layer of the esophagus consists of an outer layer of longitudinal (longitudinal) muscle fibers that accompany the shaft of the esophagus, and the inner layer porpečnih (circular). The longitudinal fibers starting from the level of cricoid cartilage, and lowering the way down, leaving room bare circular layer on the rear wall of the cervical esophagus (Killian’s triangle), before completely cover the entire wall of the esophagus. The transverse muscle fibers start from the level of cricoid cartilage in the form of irregular circles with the ends overlapping.
The innervation of the esophagus is detached, sympathetic and parasympathetic. Sympathetic inervacja be implemented over fibers originating in the cervical and thoracic sympathetic chain celiac plexus. Parasympathetic innervation of the esophagus is provided by the vagal nerve. The innervation of the wall of the esophagus is distributed through a dense network of nerve fibers in Auerbach’s, localized between the longitudinal and transverse muscle layer, and Meissner’s plexus in the submucosal tissue.
The junction between the esophagus and the stomach is a very special and zagonentu specificity of the human body. This region, known as ezofagogastrični crossing (EEA) consists of the lower esophageal sphincter (DES) and surrounding anatomical structures: diaphragm and membrane frenoezofagealne. These elements have the primary role in preventing the return of gastric contents into esophagus, while at the same time unetoj food and liquids provide a smooth passage. In addition to these basic physiological functions, I EEA must be able to obtain and retrograde passage of gastric contents into the esophagus during burping or vomiting. This seemingly simple but in fact very complicated task to enable the existence of elevated pressure the EEA. The main function of the zone of high pressure is that the connection between the esophagus and stomach to be constantly closed, but also that it is able to open in order to allow proper passage of food.
The stomach is the expanded part of the digestive tract located between the esophagus and duodenum. Anatomical stands five parts of the stomach: cardia, the relationship I pass the esophagus into the stomach, fundus, extended, most proximal part, the corpus or body of the stomach, antrum and pylorus, which is a transitional zone between the stomach and duodenum. Its shape is reminiscent of the stomach letter J or vertically laid the hook and may vary longer vertical part (cardia, fundus and corpus) and horizontal (antrum and pylorus) that each smaller part of town right corner. Clearly distinguish the front and back walls of the stomach and large and small curves. Stomach wall is constructed of four layers of the mucosa, submucosa, muscularis and serosa. The stomach is located in the upper abdomen below the left dome of the diaphragm. Clouds covered the left costal margin and partly in the upper central part of the abdomen, called epigastrium. Vascularization of the stomach is extremely rich and persistent. In parallel with vascular network mainly covers richly branched lymphatic network. Nerve wanderer (trunks) provides parasympathetic innervation that stimulates the motor function and secretion of the stomach, while the sympathetic nerves go to splahnični nerve and celiac ganglion and then follow the arterial system to the stomach.
Duodenum begins from the pylorus and ends at duodenojejunal transition, defined as Treitz’s ligament. It is divided into four anatomic areas: 1) bulb, the initial extended segment; 2) descending a downstream segment (in the middle of his medial wall through Vater’s papilla to flow into the main line and pancreatic main bile duct); 3) Horizontal (front in the form of pliers intersect the upper mesenteric vessels) and 4) upward or ascending portion. Duodenum in a frame surrounding the head of the pancreas. The duodenum is in short intervals displaces, through K + channel, lower germ chyme which is mixed with bile and pancreatic juices which allows adequate digestion.
Physiology
Welding is a process that implies fragmentation and breakdown of food to enough small parts that our body can later use to build and maintain cells and provides energy for the body. Digestion begins in the mouth and ends in the small intestine where the fully processed products ingested food are absorbed into the bloodstream. Digestion involves chewing food, the passage of food through the digestive tract, and its chemical decomposition of large molecules in sitnnije. Food and liquid through the digestive tract run special undulating movements called peristalsis.
Start welding means the act of swallowing. The first phase of the act of swallowing is consciously controlled movement, but the further course of food intake takes place through a series of reflex mechanisms. The first phase of the act of swallowing is an oral phase. After entering the bites, the food is chewed and mixed with saliva. After that, the bolus of food is of her tongue moves into the pharynx (oropharynx and hypopharynx) when performing the pharyngeal stage of swallowing. This is where conscious control of food and fluid intake, and further control the swallowing reflex is being implemented. Pharyngeal stage of swallowing takes about 1.5 seconds, during which causes the lifting of the soft palate and epiglottis time moving backwards, thereby closing the entrance to the larynx.
After swallowing pharyngeal phase begins esophageal phase. This phase begins with relaxation GES and the food quickly into the cervical esophagus and go through its shrinkage (contraction). This contraction is then transmitted as a peristaltic wave along the body of the esophagus, further suppressing a morsel of food the way down. The body of the esophagus functions as a propulsive pump to the primary role that the bolus of food put into the stomach, where overcomes the pressure gradient between the esophagus and the stomach. Esophageal peristaltic activity is reflected in the progressive contraction that is transmitted through the body of the esophagus. During this process uzudužni layer of muscles contract and shorten, thus creating the basis for the activity of the circular muscle that provide peristaltic wave.
At the turn of the esophagus to the stomach is a muscular ring structure that is called the lower esophageal sphincter (DES). To complete adequate esophageal phase of swallowing is necessary timely and complete relaxation DES. When food passes through the esophagus, the muscle relaxes and allows for a smooth passage of food into the stomach. On the other hand, it allows the gastric and duodenal content to penetrate from the stomach into the esophagus. DES can be defined as a region in which the present contraction in the level of esophagogastric transition (EEA), in the form of functional zones of high pressure final part of the esophagus. The normal basal pressure at the level of DES is about 25 mmHg. DES functionally consists of two parts: internal (muscles EEA) and outer (diaphragm), which depends on the respiratory activity. The main function of the DES is the prevention of gastroesophageal reflux disease, while he during the act of swallowing and timely relaxes completely. This relaxation DES takes between 8 and 10 seconds, which remains after by re-contraction and represents the completion of peristaltic activity of the body of the esophagus.
Primary esophageal peristalsis peristaltic reflex represents the contraction that occurs after the act of swallowing. It includes all the phases of starting oral ingestion, followed by the pharyngeal phase, followed by relaxation GES peristaltičkog wave body of the esophagus and relaxation DES. Peristaltic contractions in the body lumen of the esophagus closes and last from 2 -7 seconds, beginning in the mouth, pharynx and esophagus to continue at a rate of 2 to 4 cm / second. It should be between 10 and 15 seconds to complete the primary peristaltic activity, that is, that carried out by the bolus of food from the mouth to the stomach.
Secondary peristalsis of the esophagus does not include the act of swallowing and occurs in response to the presence of residual contents in the esophagus, or the returned content from the stomach. Contraction amplitude and velocity of propagation of the contraction waves are similar in primary contraction, but the act of pharyngeal contraction and relaxation GES absent. The aim of secondary peristalsis represents the elimination of residual or reflux contents from the esophagus.
In the stomach, food is stored, blended and then actively transported into the duodenum, where this further digested food is broken down by enzymes in the liver and pancreas. In the small intestine the food is decomposed series of chemical processes that are backed by the juices from the pancreas (pancreatic cancer) and liver. The main function of the stomach is the accumulation of ingested food and its chemical and mechanical preparation for digestion in the small intestine, and can be divided into motor and secretory. Motor functions of the stomach is threefold: 1) storing large amounts of food as long as it does not exceed the duodenum, 2) mixing food with gastric secretions to polutečnog condition called chyme and 3) slow emptying of food from the stomach into the small intestine is suitable for the digestion and absorption in the small intestine.
Gastric mucosa contains numerous cells that secrete substances necessary for the digestion of food and protection sluznokože. In the stomach, the lights are hydrochloric acid (HCl) and an internal factor (essential for the absorption of vitamin B 12), as well as the pepsinogen, mucus, and gastrin, which plays a key role in the control of gastric secretion. HCI has a multiple role: it helps digestion of protein denaturing and their activation Pepsinogen in pepsin, bactericidal, dissolved salts kacijuma and iron from food and enables their absorption. In the presence of HCl to pepsinogen to pepsin is transformed into the active proteolytic enzyme, which is and which together with the hydrochloric acid starting protein digestion in the stomach. Viscous mucus or mucus lining the gastric mucosa in the form of a gelatinous layer and the main protection of the wall of the stomach and also facilitates the slipping and food.
Daily gastric secretion is about 1500 ml. The main factors that stimulate gastric secretion of acetylcholine, histamine and gastrin. The secretion of the gastric contents is carried out through three phases: the cephalic, the gastric and intestinal phase, which overlap each other. Cephalic phase of secretion of HCl occurs before food enters the stomach and is due to observing, smelling or tasting food. Gastric occurs when food enters the stomach and is responsible for the largest part of the total gastric secretion and the resulting activation of certain reflex mechanisms and the effect of gastrin. Intestinal phase performance partly because of smaller amounts of gastrin, which is secreted into the duodenum, then in response to stretch hoses and certain chemical stimuli.
Diseases
- Anatomy and Physiology of the Foregut
- Gastroesophageal Reflux Disease (GERD)
- Barrett’s Esophagus
- Hiatal Hernias
- Achalasia
- Esophageal Motility Disorders
- Esophageal Diverticula
- Helicobacter pylori gastritis
- Peptic Ulcer Disease (PUD)
- Gallstones (Cholelithiasis)
Lexicon
Patients Informations
Soon
If you have more questions contact us:
info@refluxcentar.com

 српски
српски