Barrett’s Esophagus
Barrett’s esophagus represents a complication of gastroesophageal reflux disease, which can be described as the emergence of a special kind of mucous membrane in the esophagus resulting from chronic reflux of gastric contents into the esophagus. The clinical significance of Barrett’s esophagus is the fact that this mucous membranes genetically unstable, and prone to transformation into malignant tumors.
It is believed that about 10 – 15% of patients who suffer from GERD, eventually develop Barrett’s esophagus. Knowing what is the frequency of GERD in the general population (every fifth person), we can conclude that the prevalence of Barrett’s esophagus is very high. Although a relatively small percentage of patients develop a malignant tumor from Barrett’s esophagus (0.3 – 2%), a high prevalence of the disease tells us that if you diagnose Barrett’s esophagus, it is necessary to prisupiti monitoring and treatment, and we must act preventively.
In many countries there are recommendations to perform routine endoscopy of the upper digestive tract (sovereign method in detecting Barrett’s esophagus) in all adults aged 45 – 50 years. A number of these systematic endoscopy leads to the fact that the Barrett’s esophagus often detects and in patients who have no symptoms of GERD. This approach results in a problem and often detection of malignant tumors of the esophagus at an early stage, when the disease is still curable. Today there are very efficient methods for endoscopic removal of Barrett’s esophagus, especially endoscopic radiofrequency ablation.
The story of Barrett’s esophagus is essentially a story about the early detection, prevention, treatment and monitoring, and very serious approach to this increasingly present clinical problem.
Details about the frequency, the reasons for the emergence of, a natural progression, diagnostic methods and complications of Barrett’s esophagus, read below.
Introduction
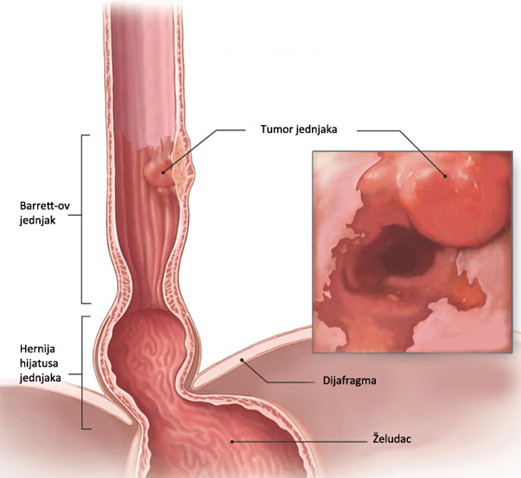
Barrett’s esophagus (BJ) is the occurrence of any specific length of metaplastic columnar epithelium that replaces pločastoslojevitu mucous membranes that normally covers the final part of the esophagus, and from which they can develop cancer. This condition occurs as a result of chronic gastroesophageal reflux disease (GERD) and predisposes the occurrence of esophageal adenocarcinoma. The concept of Barrett’s esophagus is the eponym (the name originated per person) was created by Norman Barrett in (1903-1979), the great English surgeon and one of the founders of thoracic surgery in the UK. Barrett in 1950 first described the existence of an entity cylindrical mucous membranes in the final part of the esophagus.
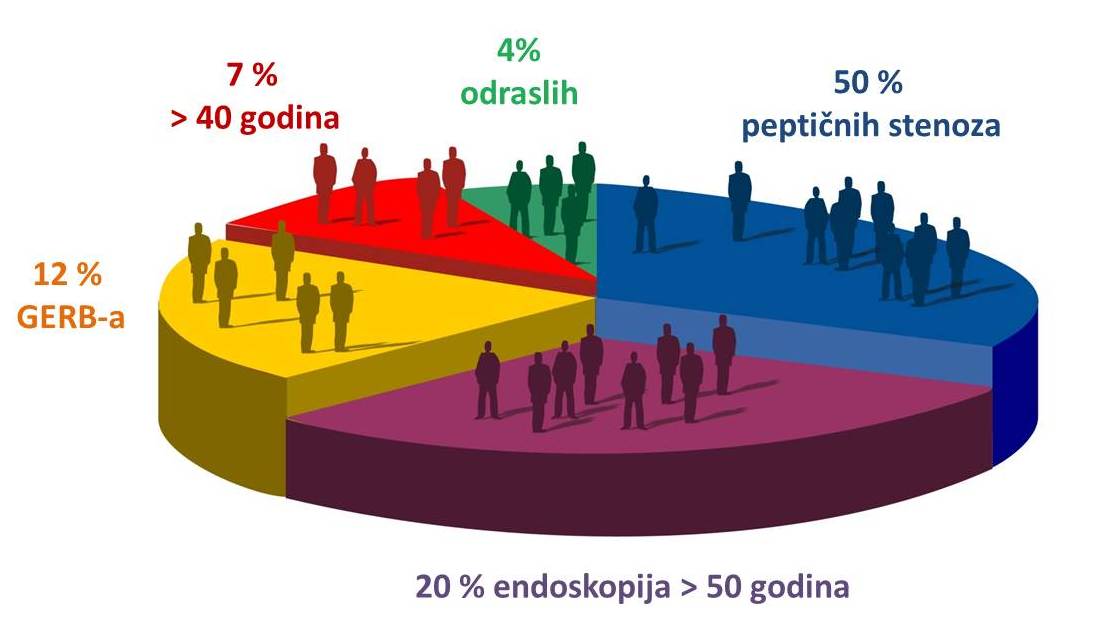
BJ is more common in developed countries still suffering from this disease 2% of the world population, or even 7% of people older than 40 years. It is estimated that in 12% of patients diagnosed with GERD there is Barrett’s esophagus. Also, in 20% of patients older than 50 years in which the ways of endoscopy for any reason, diagnosed Barrett’s esophagus. Although less than 1% of the entire population of patients with Barrett’s esophagus develop cancer, patients with BJ have about 20 times the risk of developing this disease. Adenocarcinoma of the final part of esophageal malignancy represents the fastest growing in the western world, of over 300% in the past 20 years, and is one of the most common causes of mortality among cancers.
| Risk factors for Barrett’s esophagus | |
|---|---|
| Heartburn | Symptoms of more than 10 years, larger hiatal hernia |
| Year | middle-aged and older (average age 55 years) |
| Pole | males are 3 times more, the white race |
| Lifestyle | smokers and people with obesity problems. |
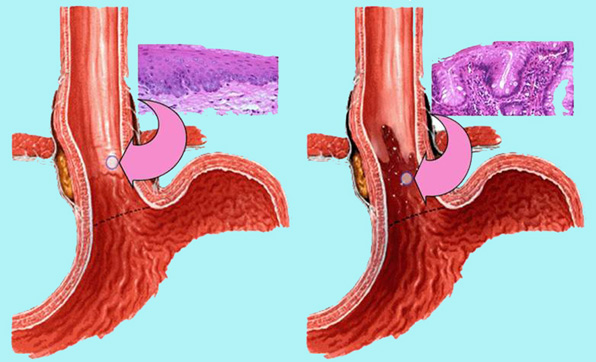
Causes
Barrett’s esophagus is diagnosed in people who have a long-standing gastroesophageal reflux disease (GERD). Over time, this damage to the constant action of gastric and duodenal contents of the lining of the lower part of the esophagus can lead to inflammation and genetic mutations that cause cell transformation. A special role in the development of Barrett’s esophagus has a content of duodenum (biliary content), which among other things owns and bile salts and lysolecithin. These ingredients duodenal contents are very harmful because while on the one hand hydrochloric acid destroys healthy pločastoslojevitu mucosa of the esophagus, bile salts such time directly affect the stem cells of the esophagus to produce another species resistant mucous membrane. Tissue final part of the esophagus takes on a different look and it is no longer the tissue of the esophagus but small intestine. This change in the tissue of the esophagus is called “intestinal metaplasia”, or Barrett’s esophagus.
The mucosa of Barrett’s esophagus is more resistant to gastric acid than normal mucous membrane of the esophagus, which indicates that such mucous membranes developed to protect’m esophagus. The problem occurs because the cylindrical cell mucosal Barrett’s esophagus have an increased risk of transformation. The clinical significance of Barrett’s esophagus is the fact that this state of precancerous lesions, ie that it can develop a malignant tumor (adenocarcinoma) the final part of the esophagus.
Symptoms
Specialized intestinal metaplasia cylindrical typical of Barrett’s esophagus does not produce any symptoms. The majority of patients with Barrett’s esophagus are initially diagnosed because of symptoms related to GERD, such as heartburn, regurgitation or dysphagia.
In patients with Barrett’s esophagus, there are significant individual differences in the perception of symptoms and the clinical picture, so consulting a doctor is always necessary when patients are perennial feeling of heartburn. The most common symptoms associated with the presence of Barrett’s esophagus are an expression of nocturnal heartburn, frequent belching and vomiting less frequently. One of the classic history data for the existence of Barrett’s esophagus is heartburn for several decades that the last few months spontaneously reduce or completely stopped. The reason for this new situation is the fact that Barrett’s mucous membranes do not possess receptors that signal the presence of acid.
In addition to the above symptoms in these patients occurs and difficulty swallowing food due Osten body esophageal peristalsis and pain in the chest and in the upper part of the stomach. Very often these patients have horničan dry cough caused by the constant return of gastric contents into the esophagus, not only but also in the bronchial tree. However, many patients with Barrett’s esophagus can be fully and asymptomatic. For the foregoing reasons, in some countries recommend routine endoscopy in all people older than 50 years. It is advised that patients who have at least once a week the symptoms of GERD present the last five years and who have many risk factors for esophageal cancer, be sure to undergo the diagnosis of suspected presence of Barrett’s esophagus. Factors which individually increase the risk of Barrett’s esophagus are older patients who are obese with a long history of heartburn .
Diagnostic
A doctor may suspect the presence of Barrett’s esophagus based on the patient’s symptoms and risk factors described above, but only the upper flexible endoscopy and biopsy can determine the right diagnosis. On the other hand, the sensitivity and specificity of radiographic examination of the esophagus due to the suspected presence of Barrett’s esophagus is very low. In order to confirm the existence of Barrett’s esophagus must be met two diagnostic criteria:
- Endoscopic must recognize the existence of the cylinder in the distal esophagus slkuzokože
- The histological examination of biopsy samples must confirm the existence of intestinal metaplasia.
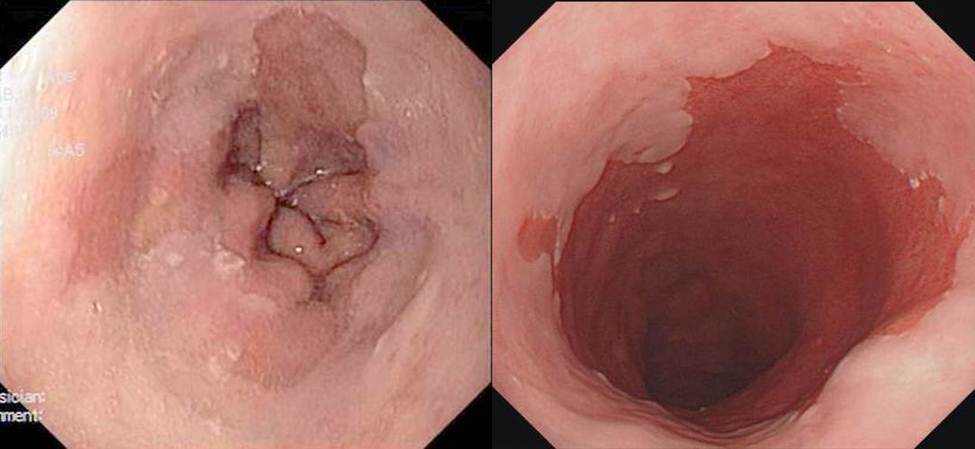
In order to document the cylindrical luzokoža on the lower part of the esophagus, endoscopist must first identify squamo-cylinder crossing, crossing mucous membranes of the esophagus in the stomach lining. In healthy subjects, the mucous membranes of the esophagus is a white, pearly and shiny, while in people with Barrett’s esophagus are pink, red and velvety. A place to meet these two types of mucous membrane called the Z line. On the other hand, the transition of the esophagus into the stomach represents an imaginary line where the anatomical ends the esophagus and the stomach begins, called ezofagogastrični crossing (EEA). EEA endoscopically identified as level najproksimalnijeg providing folds of the stomach. When skvamocilindrični crossing is above (proximal) of esophagogastric transition then there is a part of the esophagus that is covered by cylindrical mucous membranes. If the biopsy sample from this segment indicate the existence of specialized intestinal metaplasia, then diagnose Barrett’s esophagus.
State of the art endoscopes have a particularly embedded devices that enable easier identification of Barrett’s esophagus. It is always necessary to make during endoscopy biopsy sampling of tissue, with the aim of histopathological tests for the presence of Barrett’s esophagus, or confirmation of the presence of intestinal epithelium in the esophagus (intestinal metaplasia). Biopsies are taken by a strictly defined protocol from the region of the lower part of the esophagus and upper stomach. After histological examination by an experienced and specialized pathologists, there is a specific diagnosis of Barrett’s esophagus with a precisely defined TEZNO and degree of the disease.
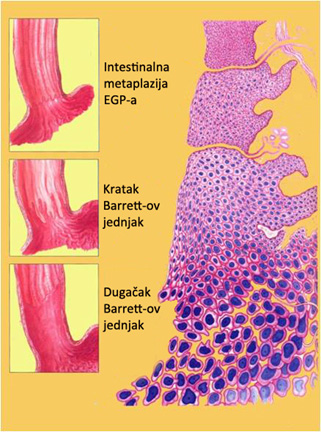
The endoscopic system of determining the size of Barrett’s esophagus called the Prague C and M criteria, is proposed to assess the presence and prevalence of Barrett’s esophagus. The criteria are based on an estimate circumferential (C value) and maximum involvement (M value) of the end of the esophagus clinidričnom mucous membrane, seen from the EEA. Endoscopic BJ also be divided into three stages and in relation to its length: long, short and intestinal metaplasia of the EEA. Barrett’s esophagus is called long when the distance between the Z lines and esophagogastritic crossing ≥3 cm and short when this distance In cases where the Z line and EEA match, and in the biopsy sample taken from Z lines are diagnosed with intestinal metaplasia, then the condition is called intestinal metaplasia of the EEA. The prevalence of a short is significantly higher than the Barrett’s esophagus long segment. Both of these conditions are often diagnosed in people older than 55 years. The overall prevalence of specialized intestinal metaplasia made out in endoscopic examination of the upper digestive tract is 13.2% with the following ratio: 1.6% long, 6.4% short Barrett’s esophagus and intestinal metaplasia 5.6% EEA. GERD associated with long Barrett’s esophagus is often complicated by ulceration of the esophagus, stenosis and bleeding. Patients with short-segment Barrett’s esophagus usually have a shorter history of mustard, and may be no symptoms of GERD. In contrast to them, patients with intestinal metaplasia EEA probably have an infection with Helicobacter pylori. The level of exposure and the mechanism of gastric acid in patients with short and long Barrett’s esophagus indicates that patients with long segment of a much stronger degree of reflux in the standing and lying down.
Complications
Najznačjanija complications of Barrett’s esophagus is that, after a while, of metaplastic cylindrical mucous membranes of the esophagus (intestinal metaplasia) may arise clear precancerous changes or dysplasia. The term “dysplasia” refers to non-specific tissue or cells irregularities, due to which they become disorganized and begin to resemble the malignant tissue or cancerous cells. According to the microscopic findings and the results of the biopsy, there are three types or “degree” Barrett’s esophagus: intestinal metaplasia (IM) without dispalazije, light dysplasia and dysplasia severe degree.
If confirmed intestinal metaplasia then begins with medication treatment, or if there are clear precancerous lesions or dysplasia, then access to such patients entirely different. Sometimes it is difficult to adequately identify precancerous histopathological changes, especially when there is inflammation caused by a pronounced reflux of gastric contents. Just for this reason it is recommended that biopsies in suspected presence of Barrett’s esophagus always ways after a while the proton pump inhibitor therapy. Dysplastic changes are divided into two major groups: the low degree of dysplasia, or significantly more severe form, a high degree of dysplasia. Although patients with all types of Barrett’s esophagus at increased risk, light and heavy dysplasia represent a subtype that carry the greatest risk to the patient. Highgrade dysplasia is itself still must be considered as the initial phase of cancer of the esophagus. It is important to understand that the progression of the initial Barrett’s esophagus (intestinal metaplasia) to cancer of the esophagus is not so frequent, and today is considered to be on an annual basis from 00:12 to 12:33% of patients develop cancer. On the other hand, for a period of four years, the relative risk of cancer of the esophagus from intestinal metaplasia is 1.1 to 3.5%. The main factors of progression of intestinal metaplasia in adenocarcinoma of the esophagus in length (relative risk 1.1% to 1 cm), presence of Barrett’s esophagus for more than 10 years (relative risk 3.2) and inflammation of the terminal part of the esophagus, esophagitis (relative risk 3.5). If to these basic factors are added age progression (˃ 50 years), male gender and obesity, they get conditions for preventive action, or remove intestinal metaplasia endoscopic procedures (read the details under radiofrekvetna endoscopic ablation of Barrett’s mucous membranes).
Tracking precancerous changes primarily intestinal metaplasia and dysplasia of low level is absolutely recommended for most patients with Barrett’s esophagus. At this point, monitoring includes regular endoscopy with biopsies noting that in the meantime taken all the possibilities of the treatment of these patients. This approach can detect precancerous changes, in terms of light or severe esophageal mucosal dysplasia, and cancer at an early stage when it can be significantly more effective treatment.
Diseases
- Anatomy and Physiology of the Foregut
- Gastroesophageal Reflux Disease (GERD)
- Barrett’s Esophagus
- Hiatal Hernias
- Achalasia
- Esophageal Motility Disorders
- Esophageal Diverticula
- Helicobacter pylori gastritis
- Peptic Ulcer Disease (PUD)
- Gallstones (Cholelithiasis)
Lexicon
Patients Informations
Soon
If you have more questions contact us:
info@refluxcentar.com

 српски
српски