Motor disorders of the esophagus represent a broad group of diseases that are manifested disturbed contractions of the esophageal body and functioning of both the upper and lower esophageal sphincter.The symptoms for this disease are very different, and can manifest sense retention, chest pain behind the breastbone and the return of stomach contents into the esophagus (regurgitation).Very often these symptoms are mistakenly attributed to heart disease or lung cancer.These disorders can not be diagnosed with certainty only with the symptoms, radiography and endoscopy are already required very precise, primarily functional diagnostic methods in order to set the correct diagnosis.
Details relating to the causes, symptomatology and dijagnstici primary motor disorders of the esophagus, read below.
When the liquid is swallowed, part goes into the lungs and are then filtered into the pericardial bag, which lubricates the feverish heart.The rest of the fluid is exhaled as vapor.
– Hippocrates (Ἱπποκράτηςc. 460 – c. 370 BC)
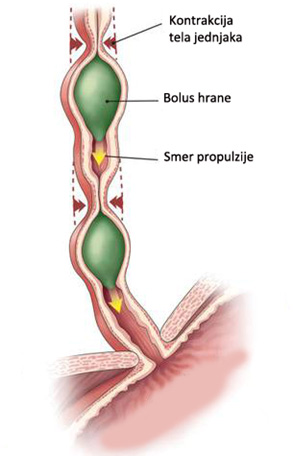
Our attitudes about the function of the esophagus have changed somewhat since Hippocrates describe what happens when ingested liquid.Taking food requires implementation of the mouth to the stomach and depends primarily on the proper functioning of the peristaltic movements of the esophagus.Disorders of esophageal peristalsis called esophageal motor disorders and include any condition for which the symptoms, especially dysphagia and chest pain, considered to be the origin neadekatnog of functioning of the esophagus.Motility disorders of the esophagus can be diagnosed with certainty only esophageal manometry.Manometry to determine the exact value of pressure in the esophageal sphincter level and their relaxation, the presence of esophageal peristalsis in the body, as well as the characteristics of peristaltic waves including their amplitude, duration, nature of repetition and the presence nepropulzivnih or partially propulsive peristaltic waves.
Although in recent years proposed several classification motility disorders of the esophagus, none of them is universally accepted.Esophageal motor disorders can be generally divided into primary and secondary.Others are due to systemic diseases such as: diajbetes, connective tissue disorders, dermatomyositis, scleroderma, amyloidosis, alcoholism, sāgas disease and various types of neoplasms (mostly adenocarcinomas of the cardia).Primary esophageal motility disorders are best classified depending on the type of disturbance of innervation of the body of the esophagus and the lower esophageal sphincter (DES).On the basis of such classification all primary esophageal motility disorders can be divided into five groups: achalasia, diffuse esophageal spasm, hiperkontraktilni esophagus, hypocontracting esophagus and nonspecific esophageal motor disorders.
CLASSIFICATION OF PRIMARY motility disorders of the esophagus
| Primary motility disorders | Manometric |
|---|---|
| Achalasia | The absence of peristalsis Inadequate relaxation and increased tone of LES |
| Diffuse esophageal spasm | Repeated or double simultaneous contractions > 20% Contractions that are not associated with the act of swallowing Amplitude> 30 mm Hg |
| Hipercontractile esophagus | Hypertensive “nutcracker esophagus” Normal peristalsis – high amplitude (> 180 mmHg) Prolonged amplitude duration (> 6 s) Hypertensive lower esophageal sphincter LES basal pressure > 45mmHg Incomplete LES relaxation |
| Hypocontractile esophagus | Inefektivni esophageal motility > 30% low amplitude contractions (<30mmHg) Nonpropulsive contractions Hypotensive LES Basal pressure <10mmHg |
| Non-specific disorders | Incomplete LES relaxation Nonpropulsive contractions > 20% Retrograde weak contractions |
In addition to the above, and today is still the most common classifications of motility disorders of the esophagus, the last couple of years the Chicago and classification based on high-resolution manometry, where motility disorders in more detail and more specifically classified.This applies particularly to the subgroup so far undefined disorders, or those disorders that conventional stationary esophageal manometry could be accurately classified.Special clinical significance of the Chicago classification is reflected in the division of achalasia three subtypes, because the previous practice has shown that such a division achalasia has a high predictive value assessment of the treatment.
Diffuse esophageal spasm
Diffuse esophageal spasm (DES) is defined as a contraction of the esophagus almost along its entire length and is damaging muscle peristalsis of the esophagus caused by enervation.Diffuse esophageal spasm is characterized by simultaneous neperistaltičkim repeated contractions of the smooth muscle of the esophagus with clinical manifestations of dysphagia and chest pain.Contractions of the body of the esophagus can be orderly (normotensive), reduced (hypo) or increased pressure (hypertension).DES occurs in about 5% of the patients examined for motility disorders of the esophagus and of unknown etiology.DES probably occurs due to disturbances activities propulsive contractions in the esophageal body formed after the act of swallowing, so that instead of the normal peristaltic contractions that suppress food the way forward (propulsive contractions) causes esophageal spasms of the body that do not move food (nepropulzivne contraction).In 30% of people with this disorder lower esophageal sphincter of the esophagus can also be in spasm.
The predominant symptoms are sudden DES severe pain behind the breastbone with the projection in the back, usually accompanied by symptoms disphonia for solid and liquid food.The pain occurs during swallowing, food intake, but even without it, suddenly even during sleep when the patient wakes up.These phenomena can occur in patients without a clear cause and etiology are unknown.Symptoms are usually casual and are typically non-progressive.This lack of symptomatic and manometric progression DES separates from other causes of esophageal chest pain (achalasia, esophageal cancer) and angina pectoris.Retrosternal pain in patients with DES may not be associated with the act of swallowing, can vary from mild to very pronounced with širenejm in the back and jaw, and last from a few seconds to several minutes.Dysphagia can occur during intake of solid food or liquid, and emphasized in the case that they are extremely cold or hot.The disease occurs more frequently in anksioznijih person.
The classic finding of DES, usually seen during barium radiography, where the body of the esophagus during the existence of simultaneous contraction has the appearance of “corkscrew” or “rosary”.Normal peristalsis exists in the upper third (striated muscles), and the so-called tertiary activity or pathological peristalsis has been observed in the region of the lower 2/3 of the esophagus (esophageal smooth muscle).Episodes of pain are not always associated with spasmodic contractions of the esophagus, and the patient may feel intense pain even when peristaltic activity appeared normal radiographically.
Endoscopic viewed lumen of the esophagus is usually appears normal but can be seen very strong peristaltic contractions or spasms of the esophagus body especially in the distal third.During endoscopy should pay particular attention to the presence of signs of GERD (esophagitis, ulceration or narrowing).Manometry represents the “gold standard” in diagnosing this disease.Classic abnormalities seen during esophageal manometry in patients with pathological findings DES simultaneous contraction of the body of the esophagus.For reliable diagnosis is essential the presence of simultaneous contraction in more than 20% sips during manometry examination.Manometry findings may point to the frequent, repetitive contractions of high amplitude, long-term contraction (> 6 sec.), Waves of high amplitude (> 180 mmHg), spontaneous contractions unrelated to sip.Some patients with DES can have high LES pressure with inadequate relaxation.A special subgroup of DES are patients with segmental distal esophageal spasm, which is defined by manometric presentation of simultaneous contractions but only in the distal third of the esophagus.The significance of these manometric findings in planning the length of cutting the muscle of the distal esophagus during the surgical treatment of these patients.
Hipercontractile esophagus
Within hiperkontraktilnih primary motility disorders of the esophagus separated by two distinct clinical entities: the esophagus as a nutcracker and hypertensive lower esophageal sphincter.
“The nutcracker esophagus”
“The esophagus shaped nutcracker” (nutcracker esophagus) is defined as non-kardilajni chest pain and / or dysphagia with the existence of peristaltic waves in the distal esophagus in which the mean amplitude of normal value for more than two standard deviations.The disease can only be diagnosed with certainty by manometric examination and when it was extended value of the amplitude of the distal peristaltičkog waves higher than 180 mmHg.In addition to these high amplitude contractions, all other peristaltic contractions are in their progression in the absence of simultaneous.Basal pressure of LES is usually normal but may be elevated, always followed by normal relaxation.The reason hypercontractility of the esophagus is unknown, but has been shown that the contraction of the individual high-pressure may be caused by secondary factors such as gastro-oesophageal reflux or stress.
The main symptom of patients with hiperkontraktilnim esophagus is retrostenalni pain, dysphagia while relatively rare.This disease is the most common disorder of motility in patients with non-cardiac chest pain and is present in approximately 30 to 50% of patients.Electrical connection between chest pain and esophageal hypercontractility is still unknown.Aggravating na- tional circumstances in the diagnosis of these patients is the fact that they are usually asymptomatic when performing esophageal manometry.
By definition, all patients with esophagus hiperkontraktilnim have normal peristalsis, so how peristaltic patterns are not altered by barium enema radiography usually indicate normal results.Upper endoscopy is normal or endoscopic ultrasound can show thickening of the muscular wall of the esophagus.Anxiety, depression, and dissociative disorders often diagnosed in these patients.Reference to a lot of stress and irritation of the esophagus (eg, acid reflux) suggests that these hiperkontraktilne abnormalities can be directly caused by these conditions.This disorder is the same as nutcracker esophagus Our results are highly individual therapy and generally unpredictable.
The hypertensive lower esophageal sphincter
The hypertensive lower esophageal sphincter (HDES) is a disorder that is diagnosed manometrically when there is an increased pressure on the level of LES (> 45 mmHg) with normal relaxation without associated disorders of esophageal body peristalsis.This manometric it directly differs from achalasia, that in these patients there is a normal peristaltic progression in the body of the esophagus.The optimal way of treating this disease are pneumatic dilation and ezofagokardiomiotomija and accompanying fundoplication.
Hypocontracting esophagus
Most disorders esophageal peristalsis in which motility characterized by a low amplitude simultaneous contractions of the distal esophagus, or incomplete peristalsis in which the waves do not transmit the entire length of the distal esophagus called esophageal motility inefektivni (IMJ).BUD-defined by manometric amplitude of contractions in the presence of the distal esophagus of less than 30 mm Hg, which can be seen in more than 30% contraction in the distal esophagus.Most patients with esophageal motility inefektivnim have gastroesophageal reflux disease often associated with respiratory or problems of the throat, ears and nose.Low pressure at the level of the distal esophagus and DES is often seen in patients with gastro-esophageal reflux, suggesting that hypocontracting esophagus may be a result of chronic damage to the acid of the distal esophagus.Dysphagia in these patients usually mild, while heartburn and acid regurgitation quite frequent.Severe dysphagia indicates the presence of anatomical problems such as esophagitis or peptic stricture.Treatment of these patients is mainly focused on the control of gastroesophageal reflux.
Non-specific esophageal motility disorders
The diagnosis of non-specific motility disorders of the esophagus (NPMJ) is often used in the examination of patients with dysphagia and / or chest pain who have abnormal esophageal motility are but does not meet the criteria fixed for other specific diagnosis.The only essential finding for NPMJ is an abnormality of peristalsis of sufficient gravity to establish any (other) diagnosis.The list of associated findings for NPMJ includes contractions that are retrograde, recurring, high, low amplitude, prolonged or spontaneous.Incomplete relaxation of the DES may also be seen in patients with NPMJ.These findings may be found in various combinations.Treatment NPMJ has not yet been standardized, and treatment decisions are often based on symptomatic therapy, guided by the dominant findings (spasm, hypocontractility, etc.).On the other hand, many NPMJ represent only the beginning or early stage is still incompletely differentiated primary motility disorders of the esophagus, causing regular manometric control in these patients of extreme prove significant.
Diseases
- Anatomy and Physiology of the Foregut
- Gastroesophageal Reflux Disease (GERD)
- Barrett’s Esophagus
- Hiatal Hernias
- Achalasia
- Esophageal Motility Disorders
- Esophageal Diverticula
- Helicobacter pylori gastritis
- Peptic Ulcer Disease (PUD)
- Gallstones (Cholelithiasis)
Lexicon
Patients Informations
Soon
If you have more questions contact us:
info@refluxcentar.com

 српски
српски